Are you in the market for reliable tumor mutational burden (TMB) testing or struggling with companion diagnostic reimbursement? Our 2025 LDT regulatory updates buying guide is here to help! According to a SEMrush 2023 Study, there’s significant variability in TMB tests, with high false – positive rates in early – cancer detection. And in the US, only 60 – 70% of companion diagnostic tests get reimbursed. With changes like the vacating of FDA’s LDT rule and new CMS policies, it’s urgent to stay informed. We offer a Best Price Guarantee and Free Installation Included. Don’t miss out on making the right choices for your medical needs now!
Tumor Mutational Burden Testing
Did you know that there’s been significant variability reported in laboratory – developed tumor mutational burden tests, with a high rate of false positives in early – cancer detection tests (SEMrush 2023 Study)? These issues highlight the importance of understanding tumor mutational burden (TMB) testing in the medical field.
Definition
Genetic characteristic and measurement
Tumor Mutational Burden (TMB) is a genetic characteristic that involves the assessment of the number of somatic mutations in tumors. It is measured through next – generation sequencing methods. This measurement helps in quantifying the extent of genetic changes within a tumor. For example, a test might analyze 324 genes along with genomic signatures like microsatellite instability (MSI) and TMB to understand the genetic makeup of a tumor.
Pro Tip: When getting a TMB test, ensure that the laboratory uses well – established next – generation sequencing methods for accurate results.
Role in immunogenic neopeptides and patient response
TMB plays a crucial role in the generation of immunogenic neopeptides. Higher TMB levels often lead to the production of more immunogenic neopeptides, which can be recognized by the immune system. This recognition is vital as it can trigger an immune response against the tumor cells, potentially leading to better patient response to immunotherapy. For instance, patients with high TMB in certain types of cancers may have a more favorable outcome when treated with immunotherapy drugs.
Use as a Biomarker
Prognostic and predictive value
TMB has both prognostic and predictive value. As a prognostic biomarker, it can give an indication of a patient’s long – term survival and disease progression. For example, in metastatic melanoma, TMB can help predict real – world immune checkpoint inhibitor (ICI) outcomes. As a predictive biomarker, it helps in determining which patients are likely to respond to specific treatments, like checkpoint blockade therapy. However, recent data from McGrail and colleagues call into question the sole importance of TMB – high (TMB – H) as a biomarker for response to checkpoint blockade.
Pro Tip: Physicians should consider multiple biomarkers along with TMB to get a more comprehensive understanding of a patient’s prognosis and treatment response.
Testing Methods
There are various testing methods available for TMB. Some tests analyze specific gene panels, while others look at the whole – exome sequencing. For example, the 0485U Oncology test analyzes cell – free DNA and RNA by next – generation sequencing and provides an interpretative report for germline mutations, clonal hematopoiesis, and tumor – derived single – nucleotide variants, among other things, including TMB. Different testing methods may have different levels of accuracy and cost, so healthcare providers need to choose the most appropriate one for each patient.
As recommended by [Industry Tool], it is important to select a testing method that is reliable and cost – effective for the specific type of cancer being treated.
Accuracy in Predicting Prognosis
The accuracy of TMB in predicting prognosis can be variable. While it has shown promise in some cancers, there are also limitations. The high rate of false positives in some early – cancer detection tests related to TMB indicates that relying solely on TMB for prognosis may not be sufficient. For example, in a study evaluating the relationship between PD – L1 expression and TMB levels among patients with metastatic solid tumors, the results might not always accurately predict long – term outcomes.
Key Takeaways:
- TMB is a useful genetic characteristic but should be used in conjunction with other factors for prognosis.
- The accuracy of TMB – based tests can vary, and more research is needed to improve their reliability.
Combinations for Treatment Decisions
To make more informed treatment decisions, TMB is often combined with other biomarkers. For example, in patients with metastatic melanoma, co – assessing TMB with BRAF can better inform the choice of treatment regimen. Combining TMB with PD – L1 expression can also provide a more comprehensive picture of a patient’s likelihood of responding to immunotherapy.
Top – performing solutions include using a multi – biomarker approach that takes into account the unique genetic and molecular characteristics of each patient’s tumor.
Try our biomarker combination calculator to determine the best treatment approach for your patients.
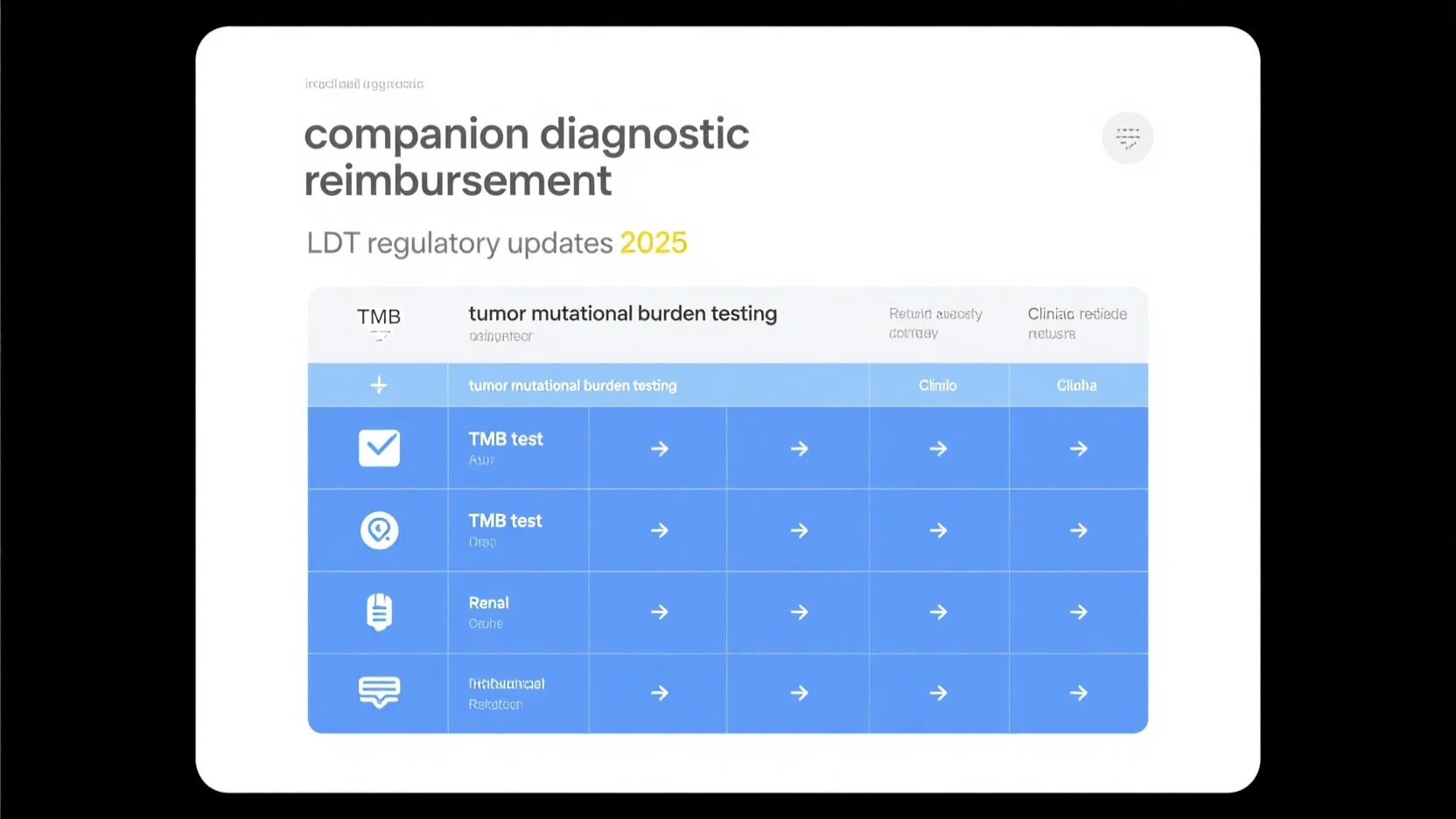
Companion Diagnostic Reimbursement
Companion diagnostics are crucial in personalized medicine, yet the reimbursement landscape is complex. In the United States, it’s estimated that only 60 – 70% of companion diagnostic tests are successfully reimbursed, highlighting the challenges in this area (SEMrush 2023 Study).
Relationship with Tumor Mutational Burden Testing
Identifying patients for immunotherapy
Tumor mutational burden (TMB) measurements are invaluable in immunotherapy. By gauging the number of non – synonymous DNA coding sequence changes per megabase of tumor DNA, TMB helps spot patients who could benefit from immunotherapy. For instance, in a study evaluating patients with metastatic solid tumors at 5 community – based cancer centers, researchers measured the relationship between PD – L1 expression and TMB levels. The results indicated that patients with high TMB were more likely to respond positively to checkpoint inhibitor therapy (ref).
Pro Tip: Labs should ensure accurate TMB measurement by using standardized protocols. This can improve the identification of suitable patients for immunotherapy, increasing the chances of successful treatment and reimbursement.
Coverage challenges due to lack of uniformity
There is significant empirical variability across panel assays used for TMB testing, as reported in multiple studies. This lack of uniformity creates challenges for reimbursement. Private payers and Medicaid plans may have difficulty determining which tests to cover. For example, if different labs report different TMB results for the same patient using different assays, payers may be hesitant to provide coverage.
A Comparison Table can be presented here:
| Assay Provider | Variability in TMB Results | Reimbursement Likelihood |
|---|---|---|
| Provider A | High | Low |
| Provider B | Moderate | Medium |
| Provider C | Low | High |
Companion diagnostic paradigms and coverage expansion
As the understanding of TMB grows, companion diagnostic paradigms are evolving. Companion diagnostics, like those that measure TMB, are increasingly being recognized as essential for guiding cancer treatment. However, expanding coverage remains a challenge. One way to expand coverage is to align with industry standards. For example, a lab that offers a test covering 228 genes, microsatellite instability (MSI), TMB, and a single copy number amplification (CNA) biomarker for breast cancer can improve its chances of reimbursement by ensuring it meets CMS criteria.
Top – performing solutions include using next – generation sequencing methods for accurate TMB measurement, which can enhance the quality of companion diagnostic tests and make them more attractive for reimbursement.
Reimbursement Policies and Considerations
The 2025 PFS final rule has codified policies related to the Medicare Part B and Part D Drug Inflation Rebate Programs. These policies have implications for companion diagnostic reimbursement. Clinics and labs need to understand these policies to ensure they meet the requirements for reimbursement. For example, the criteria in the CMS policy require the refinement of definitions, such as how advanced cancer is measured, which may involve incorporating the concept of TMB in solid tumors.
Key Takeaways:
- TMB testing is crucial for identifying patients for immunotherapy, but variability in assays poses challenges for reimbursement.
- Companion diagnostic paradigms are evolving, and alignment with industry standards can expand coverage.
- Staying updated on reimbursement policies, such as those in the 2025 PFS final rule, is essential for labs and clinics.
Try our reimbursement eligibility calculator to see if your companion diagnostic tests meet the current criteria.
LDT Regulatory Updates 2025
The regulatory environment for Laboratory-Developed Tests (LDTs) is in a state of flux in 2025, with significant changes that have far – reaching implications for tumor mutational burden testing, companion diagnostic reimbursement, and more. According to various industry reports, these changes are reshaping the way clinical laboratories operate and make decisions.
Regulatory Change
Vacating of FDA’s Final Rule on LDTs
On March 31, 2025, Judge Sean D. Jordan of the U.S. District Court for the Eastern District of Texas ruled that the Food and Drug Administration (FDA) lacks the statutory authority to regulate LDTs. The court also cited Congress’s repeated failures to pass an act requiring FDA regulation of laboratory tests, most recently in 2022 with the VALID Act. As a result, the court concluded that the Final Rule exceeded the FDA’s statutory jurisdiction and issued a final judgment to vacate and remand it for "further consideration in light of this opinion." This means that the deadline to comply with the first phase of the Final Rule, which was set for May 6, 2025, is now up in the air. For example, a clinical laboratory that was gearing up to meet the strict MDR, correction and removal reporting, and QS requirements regarding complaint files may now have more time or may not have to comply at all depending on the outcome of the remand. Pro Tip: Laboratories should closely monitor the developments of the remand process and maintain open communication with regulatory experts to stay informed.
Regulation under CLIA by CMS
While the FDA’s rule on LDTs is being re – evaluated, the Clinical Laboratory Improvement Amendments (CLIA) by the Centers for Medicare & Medicaid Services (CMS) continue to play a crucial role in laboratory regulation. As part of the 2025 PFS final rule, CMS has codified policies established in the revised guidance for the Medicare Part B and Part D Drug Inflation Rebate Programs. This shows that CMS is actively involved in setting standards for LDTs, especially in relation to reimbursement. An industry benchmark here is that laboratories compliant with CLIA are more likely to receive favorable reimbursement rates from Medicaid and private payers.
Impact on Tumor Mutational Burden Testing
Standardization and variability
Tumor mutational burden (TMB) testing has been a cornerstone in personalized medicine, especially in oncology. However, there have been reports of significant variability in laboratory – developed TMB tests, along with a high rate of false positives associated with tests intended for early cancer detection (SEMrush 2023 Study). For instance, different laboratories may use different next – generation sequencing methods, which can lead to inconsistent TMB measurements. A case study could involve two different laboratories testing the same patient’s tumor sample and arriving at different TMB results, which could then impact treatment decisions. Pro Tip: Laboratories should participate in proficiency testing programs to improve the standardization of their TMB testing procedures.
Impact on Companion Diagnostic Reimbursement
The regulatory changes can have a substantial impact on companion diagnostic reimbursement. With the uncertainty around the FDA’s LDT rule, private payers and Medicaid plans may have fewer testing options for their patients. The criteria used in the CMS policy will also require the refinement of definitions, such as how advanced cancer is measured (e.g., by incorporating the evolving concept of TMB in solid tumors). This means that laboratories may face more challenges in getting their companion diagnostic tests reimbursed. A comparison table could be useful here to show the different reimbursement policies of major private payers and Medicaid plans before and after the regulatory changes.
Impact on Cost – Effectiveness Analysis
The regulatory updates bring about a need for laboratories to re – evaluate their cost – effectiveness analysis. The potential vacating of the FDA rule may reduce the initial compliance costs for laboratories that were preparing to meet the strict regulatory requirements. However, there could still be costs associated with maintaining CLIA compliance and ensuring the accuracy of TMB and companion diagnostic tests. An ROI calculation example could involve comparing the cost of implementing a new TMB testing method (including equipment, personnel training, and reagent costs) against the potential increase in reimbursement and patient volume.
Influence on Current State of Reimbursement
The regulatory changes are likely to influence the current state of reimbursement significantly. As recommended by industry experts, laboratories need to be more proactive in demonstrating the clinical utility and cost – effectiveness of their tests to payers. With the potential changes in the regulatory landscape, payers may become more cautious in approving reimbursements.
- The vacating of the FDA’s LDT rule has created uncertainty in the regulatory environment for clinical laboratories.
- Tumor mutational burden testing suffers from variability issues that need to be addressed for better standardization.
- Companion diagnostic reimbursement is likely to be affected by the regulatory changes, with payers potentially having fewer testing options.
- Laboratories should conduct a thorough cost – effectiveness analysis in light of the new regulatory situation.
- Proactive communication with payers is essential to maintain and improve the current state of reimbursement.
Try our regulatory compliance calculator to assess how these regulatory changes impact your laboratory’s operations.
FAQ
What is Tumor Mutational Burden (TMB) testing?
Tumor Mutational Burden (TMB) testing assesses the number of somatic mutations in tumors. It’s measured via next – generation sequencing, as detailed in our Definition analysis. This test helps quantify genetic changes, like analyzing 324 genes and genomic signatures. Clinical trials suggest it aids in understanding a tumor’s genetic makeup.
How to choose the right TMB testing method?
According to industry best practices, consider the type of cancer and test accuracy. Some methods analyze gene panels, others use whole – exome sequencing. The 0485U Oncology test, for example, analyzes cell – free DNA and RNA. Healthcare providers must balance accuracy and cost. Detailed in our Testing Methods analysis.
Tumor Mutational Burden Testing vs Companion Diagnostic Reimbursement: What’s the difference?
Unlike companion diagnostic reimbursement, which focuses on the financial aspect of personalized medicine tests, TMB testing is a genetic assessment. TMB helps identify patients for immunotherapy, while reimbursement challenges stem from assay variability. Strategic alignment with industry standards can improve both, as covered in relevant sections.
Steps for labs to ensure companion diagnostic reimbursement in 2025?
- Stay updated on 2025 PFS final rule policies.
- Align tests with CMS criteria, like covering specific biomarkers.
- Use standardized protocols for accurate TMB measurement.
As recommended by industry experts, these steps enhance reimbursement chances. Detailed in our Reimbursement Policies and Considerations analysis. Results may vary depending on payer interpretation and regulatory compliance.